Introduction:
In recent months, reports of new Nipah virus cases from India have once again raised public concern across South Asia. For countries like Nepal, which share open borders, frequent travel, and similar environmental conditions with India, awareness becomes especially important. Although Nipah virus infections are rare, they are among the most lethal viral diseases known to affect humans.
From a microbiology and public health perspective, sharing accurate, evidence-based information is essential. This article provides a clear and practical overview of the Nipah virus—its origin, transmission routes, symptoms, diagnosis, treatment options, and most importantly, preventive strategies to reduce risk.

What Is Nipah Virus?
Nipah virus (NiV) is a zoonotic virus, meaning it is transmitted from animals to humans. It belongs to the Henipavirus genus within the Paramyxoviridae family. The virus was first identified during a major outbreak in Malaysia in 1998–1999, where it primarily affected pig farmers and resulted in a high number of deaths.
The natural hosts of Nipah virus are fruit bats of the Pteropus genus, commonly known as flying foxes. These bats can carry the virus without appearing ill, allowing the pathogen to circulate silently in nature and occasionally spill over into humans and domestic animals.
Why Is Nipah Virus Considered Extremely Dangerous ?
Nipah virus poses a serious global health threat due to several critical factors:
- Very high fatality rate, ranging from 40% to 75%
- No approved antiviral treatment
- No licensed human vaccine
- Ability to spread from person to person
- Severe damage to the brain and respiratory system
- Sudden and unpredictable outbreaks
Because of these characteristics, the World Health Organization (WHO) has classified Nipah virus as a priority pathogen with epidemic potential.
Modes of Transmission
Nipah virus spreads through close contact with infected animals, contaminated food products, or infected individuals.
1. Animal-to-Human Transmission
Humans can become infected when they come into contact with materials contaminated by fruit bats, such as:
- Fruits contaminated with bat saliva, urine, or feces
- Raw or unprocessed date palm sap
Infection can occur through:
- Eating partially eaten or fallen fruits
- Drinking fresh date palm sap
Handling infected pigs or other animals
2. Human-to-Human Transmission
Person-to-person spread has been documented, particularly during outbreaks in India and Bangladesh. Transmission occurs through:
- Close physical contact with infected individuals
- Exposure to respiratory droplets
- Contact with blood, saliva, urine, or other body fluids
Healthcare settings are especially vulnerable when proper infection control measures are not strictly followed.
Countries Where Nipah Virus Has Been Reported
Confirmed outbreaks of Nipah virus have occurred mainly in:
- Malaysia
- Bangladesh
- India (especially Kerala and nearby regions)
Although Nepal has not officially reported any cases so far, its geographical proximity, shared bat species, and cross-border movement highlight the importance of preparedness and surveillance.
Incubation Period
The incubation period typically ranges from 4 to 14 days, but in some individuals, symptoms may appear as late as 45 days after exposure. This prolonged incubation makes early detection and outbreak control more challenging.
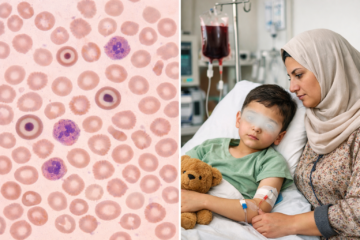
Clinical Signs and Symptoms
The severity of Nipah virus infection can vary widely.
Early Symptoms
- Fever
- Headache
- Muscle aches
- Sore throat
- Vomiting
- General weakness
Respiratory Symptoms
- Persistent cough
- Shortness of breath
- Acute respiratory distress
Neurological Symptoms (Severe and Life-Threatening)
- Dizziness
- Confusion or altered mental status
- Seizures
- Encephalitis (inflammation of the brain)
- Rapid progression to coma within 24–48 hours in severe cases
Diagnosis of Nipah Virus Infection
Early laboratory confirmation is essential for patient management and outbreak control.
Diagnostic Methods Include:
- RT-PCR to detect viral genetic material
- ELISA tests for IgM and IgG antibodies
- Virus isolation (performed only in specialized laboratories)
Commonly Tested Samples:
- Blood
- Throat or nasal swabs
- Cerebrospinal fluid (CSF)
- Urine
Due to its extreme risk, Nipah virus testing must be conducted in biosafety level-4 (BSL-4) laboratories.
Treatment and Clinical Management
At present, there is no specific antiviral drug approved for treating Nipah virus infection.
Treatment focuses on supportive care, which includes:
- Intensive care monitoring
- Oxygen therapy or mechanical ventilation
- Management of fever and seizures
- Maintenance of fluid and electrolyte balance
Some antiviral medications, such as Ribavirin, have been used on an experimental basis, but their effectiveness remains uncertain.
At present, there is no specific antiviral drug approved for treating Nipah virus infection.
Treatment focuses on supportive care, which includes:
- Intensive care monitoring
- Oxygen therapy or mechanical ventilation
- Management of fever and seizures
- Maintenance of fluid and electrolyte balance
Some antiviral medications, such as Ribavirin, have been used on an experimental basis, but their effectiveness remains uncertain.
Prevention and Control Strategies
Since treatment options are limited, prevention is the most effective defense against Nipah virus.
1. Food Safety Practices
- Avoid consuming fruits that appear bitten or damaged
- Wash fruits thoroughly before eating
- Do not drink raw date palm sap
Cover sap collection containers to prevent bat contamination
2. Safe Animal Handling
- Avoid contact with sick or dead animals
- Use gloves and protective clothing when handling animals
- Report unusual animal illnesses or deaths promptly
3. Infection Control in Healthcare Facilities
- Use appropriate personal protective equipment (PPE)
- Isolate suspected or confirmed patients
- Maintain strict hand hygiene
- Dispose of medical waste safely
4. Community Awareness
- Educate the public about bat-related transmission
- Encourage early medical consultation for symptoms
- Promote science-based information rather than fear
Role of Microbiology and Laboratory Professionals
Microbiology and laboratory experts are vital in controlling Nipah virus outbreaks through:
- Early laboratory diagnosis
- Disease surveillance
- Biosafety enforcement
- Training healthcare personnel
- Supporting public health education
Accurate and timely laboratory reporting can prevent isolated cases from escalating into widespread outbreaks.
Is Nepal at Risk?
Although no confirmed cases have been reported in Nepal, potential risk factors include:
- Open borders with affected regions
- Presence of fruit bat populations
- Frequent population movement
- Limited high-containment laboratory facilities
Strengthening surveillance systems, preparedness planning, and public awareness is essential.
Conclusion
Nipah virus is a rare but highly lethal zoonotic infection with serious epidemic potential. In the absence of specific treatment or vaccines, early detection, preventive measures, and public awareness remain the strongest tools to protect communities.
Being informed is not a cause for panic, it is a step toward preparedness. Through scientific understanding, responsible behavior, and strong healthcare systems, the threat posed by Nipah virus can be effectively minimized.
Frequently Asked Questions (FAQs)
What is Nipah virus?
Nipah virus (NiV) is a serious zoonotic virus that spreads from animals to humans. It can cause severe respiratory illness and brain inflammation (encephalitis) and has a high death rate in some outbreaks.
How does Nipah virus spread to humans?
Nipah virus spreads mainly through:
- Direct contact with infected bats or pigs.
- Eating raw date palm sap or fruits contaminated by bats.
- Close contact with infected humans, especially body fluids like saliva or respiratory droplets.
What are the common symptoms of Nipah virus infection?
Symptoms usually appear 4–14 days after exposure and may include:
- Fever and headache
- Muscle pain and weakness
- Vomiting and sore throat
- Difficulty breathing
- Drowsiness or confusion
- Seizures and loss of consciousness in severe cases
How dangerous is Nipah virus?
Nipah virus is considered very dangerous because:
- It has a high fatality rate.
- There is no specific cure or vaccine yet.
- It can cause rapid neurological complications.
Early medical care greatly improves survival chances.
Is there a cure for Nipah virus?
No. Currently, there is no specific antiviral cure for Nipah virus. Treatment is supportive, focusing on:
- Managing symptoms.
- Providing respiratory support.
Preventing secondary infections.
Is there a vaccine available for Nipah virus?
As of now, no approved vaccine is available for public use. However, several vaccines are under research and clinical trials.
What types of samples are used for Nipah virus testing?
Laboratory testing may use samples such as:
- Throat or nasal swabs
- Blood samples
- Urine samples
- Cerebrospinal fluid (CSF) in severe cases
The choice of sample depends on the stage and severity of the illness.
Why is strict laboratory safety important during Nipah virus testing?
Because Nipah virus is highly infectious:
- There is a risk of laboratory-acquired infection.
- Strict biosafety protocols protect laboratory staff and the community.
When should Nipah virus laboratory testing be done?
Testing should be done immediately if a person has:
- High fever with neurological symptoms.
- History of contact with infected persons or animals.
- Travel or residence in an outbreak-affected area.
Early testing is critical for patient care and outbreak control.